curiousKC | Answers to COVID Questions You Need to Know Your Questions Are Welcome
Published May 10th, 2022 at 6:00 AM
Above image credit: Questions about COVID-19 abound. Here's what our team of reporters knows so far. (Adobe)Editor’s note: Flatland’s public-powered tool curiousKC is here to keep you updated. So, here are answers to some of your most frequently asked questions about the COVID-19 pandemic. These answers are summaries based on the information in each linked article.
Last updated: 5/10/2022
Q: What’s the infection rate as of May?
At the moment, infection rates are estimated to be low in the Kansas City metro area, at least Kansas-side figures show, according to available data. It’s important to note that experts believe COVID cases are undercounted, so this is an estimate. Context is also important, which you’ll learn more about in the following answers. Cases are on the rise across the U.S.
Missouri stopped updating its data at the county level in May. However, local nonprofit newsrooms such as KC Media Collective partner The Beacon continues pumping out a COVID Dashboard to help keep folks informed. See that here.
Another nonprofit at the national level called COVID Act Now crunches data from partners such as Stanford Medicine, Harvard Global Health Institute and Georgetown University to create easy-to-understand charts for communities across the U.S.
Here’s what the metropolitan area looks like now:
Q: What does ‘infection rate’ mean?
This diagram from COVID Act Now helps explain. Pretend Person X has an infection rate of 3. They would likely expose three people to the virus, who – if they contract COVID-19 – will also be infectious to three more folks and so on:
Q: Are we now in an endemic state or still in a pandemic?
Experts’ opinions are all over the map. Since cases still tend to spike and with cases still rising across the U.S., some public health experts say we’re technically still in pandemic status.
Testing has shown that cases are rising in every region and among all age groups, so it is advisable to wear a mask around folks who may be vulnerable or at risk for complications.
“Rising test positivity indicates that there is more disease in the community than what current test capacity can adequately monitor. In other words, there’s a lot of disease spreading in those 65+ that we can’t see,” wrote Amber Schmidtke, a Ph.D. in medical microbiology and immunology. Schmidtke publishes the COVID Digest, touching on key trends folks should pay attention to.
On May 5, the focus was on 1 million COVID deaths in the United States. She urged folks to stay vigilant and to remind readers this virus has caused and is still causing serious disease.
“We are well underway in the next wave of illness and the country has abandoned all efforts to stop it. How many more unnecessary deaths will result from this apathy?” she wrote.
Q: What is the CDC doing now to improve the public’s trust?
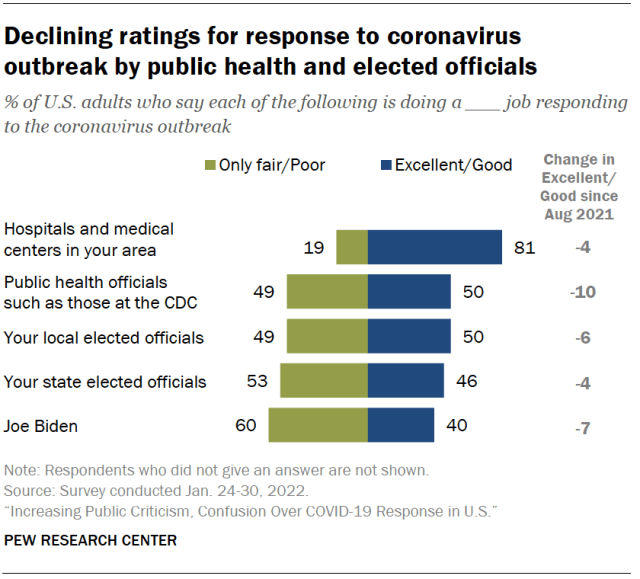
For context, various studies show that the public’s perception of public health, government leaders and institutions is poor and worsening.
A Harvard poll showed that only half of U.S. respondents trust the Centers for Disease Control and Prevention. State and local health departments didn’t fare any better, according to NPR. This Pew report showed the same trend.
Distrust and the inconsistent messaging were at the center of conversation during an April meeting of health leaders at Harvard’s public health school entitled “CDC At the Crossroads.” The consensus was a need for transprency and collaboration between health and government agencies.
Former CDC directors who were in attendance expressed a need for politicians to work with public health workers and science communicators to repair the public’s waning distrust.
Here are a few key quotes that sums up that webinar’s takeaways:
- Robert Redfield, Senior Medical Advisor at PersOwn/CDC Director from 2018 to 2021: “I had idolized CDC for my 30-year medical career thinking this was the top of the top and to find out how under-resourced they are … This is why I said to you, one of my most important priorities is that our nation invest proportionately to CDC and public health.”
- Bill Foege, Physician and Epidemiologist/CDC Director from 1977 to 1983: “Public health is totally dependent on politics … Our question should be how do we incorporate politicians in the solutions so they see themselves as part of the solution and not just a place to give money.”
- Dr. Bill Roper, Professor of Medicine and Public Health, University of North Carolina/CDC Director, 1990 to 1993: “We need science, the best of science to guide the decisions that are made by political leaders to implement effective public health programs. We need those two things to work together for public health to be successful.”
Q: What do I need to know about COVID-19 more than two years in? Is it still a threat?
The virus is still a threat to public health, particularly for the roughly 7% of the population that is immunocompromised. Though local governments have removed certain restrictions, the virus is still infecting folks, particularly those 65 and older, and causing hospitalizations. Plus, reinfections are happening.
This doesn’t begin to cover new issues folks with long COVID are facing.
Keep in mind that case incidences have risen around 22% in the past seven days, according to the most recent Community Profile Report, which you can see here. The virus is still very much around but we can continue to mask up, test and trace cases among our social circles.
“I’m asking you to please notice,” Schmidtke pleas at the end of her COVID Digest newsletter.
Q: What do we need to know about vaccine, infection and hospitalization rates in the Kansas City area?
At the moment nearly 60% of residents are fully vaccinated, which includes boosters. However, medical experts are reporting a plateau in vaccinations.
According to COVID Act Now Coalition data, transmission rates remain “very high” in the Kansas City metropolitan area, with daily cases averaging 1,298 new confirmed cases per day.
Although hospitalizations are on the decline, the rate nearly tripled in January 2022 compared with January 2021. This has overburdened healthcare systems in the metro.
“Every hospital in the metro and across Kansas are still reporting staff out sick with COVID and/or awaiting test results while demand for services continues to rise,” Jill Chadwick, spokesperson for the University of Kansas Health System, said in an email.
Check out our KC Media Collective partner The Beacon’s COVID Dashboard.
Q: What’s the status of vaccines for children younger than 5 years of age?
In December, Pfizer-BioNTech had submitted a request for emergency use authorization for a long awaited vaccine for infants through 4 years old.
On Feb. 11, the Federal and Drug Administration (FDA) announced it needed more time to evaluate new data from the three-dose clinical trials of a Pfizer-BioNTech COVID-19 Vaccine. Initially, the FDA wanted to roll out a vaccine for the youngest members of the population by Feb. 21.
The clinical trials are gathering data on a three-dose vaccine, but early trial results “fell short,” according to Reuters.
In light of new clinical trial results, Dr. Janet Woodcock, acting commissioner of the FDA, and Dr. Peter Marks, director of the Center for Biologics Evaluation and Research (CBER), shared the following joint statement about why the agency decided to delay review: “The agency will ensure the data support effectiveness and safety before authorizing a COVID-19 vaccine for use in our youngest children.”
The FDA expects new data on the third dose clinical trials in April and a possible vaccine rollout could be expected in the next few months, according to the FDA release.
Q: What do we need to know about the omicron variant?
In November 2021, the World Health Organization (WHO) identified a new variant and called it “omicron.”
It was considered a “variant of concern,” which the Centers for Disease Control and Prevention (CDC) define as “a variant for which there is evidence of an increase in transmissibility, more severe disease (for example, increased hospitalizations or deaths), significant reduction in neutralization by antibodies generated during previous infection or vaccination, reduced effectiveness of treatments or vaccines, or diagnostic detection failures.”
Several key takeaways are:
- Omicron is still COVID and it is still dangerous.
- Evidence shows that the omicron variant is more contagious.
- Even if an infected person’s symptoms are mild, the long-lasting effects of the illness are cause for concern.
- Omicron is detectable on Polymerase Chain Reaction (PCR) tests but experts are still learning more about at-home tests.
- Experts are concerned about the most recent surge and the ever-increasing disability due to long COVID.
- Hospitals saw a spike in hospitalizations and are already overwhelmed, buckling under pressure, according to the Medical News Network
“The situation that we’re in with the omicron variant, unfortunately, is in many cases, a man-made phenomenon,” said Jessica Malaty Rivera, an infectious disease epidemiologist and science communicator who was previously with the COVID Tracking Project.
Omicron, she said, is affecting vaccinated and unvaccinated folks across the globe. Malaty Rivera explained that this phenomenon is important to view in the context of vaccine access and equity. Variants emerge and replicate when they go unchecked.
That is why experts like her urge getting vaccinated and work toward informing the public about these viruses.
“When we say things like, ‘No one is safe until everyone is safe,’ that has a direct correlation to what we’re talking about here in the context of variants and vaccine equity,” she added.
“Each individual choice has a direct impact on how our systems and how our communities can actually exist and then function normally. … We have taken way too long to get many countries first and second doses while we are here in the United States (with) many of us on our third dose and even contemplating a fourth, which to me is unfathomable.”
Q: What do we need to know about long COVID?
Long COVID, or post-COVID, are lingering symptoms or newly emerging illnesses related to COVID-19 illness.
Malaty Rivera, who has been on various news shows and on her personal social media to debunk dangerous, incorrect theories, said there are too many unknowns that are cause for concern.
“It’s causing disability,” she said. “It’s causing issues of chronic illness. It’s causing issues of mental health crises … And I think that we have to remind people that the vaccines are another way to protect or reduce your risk of getting that.”
The CDC has a few resources for folks and their families, which can be found here:
Additionally, a new clinical trial led by a Kansas City physician is enrolling folks across the U.S. to study these conditions to help inform the creation of therapies that could help long COVID illness.
You can read more about that here.
Q: Why is there a “new version” of the coronavirus?
Viruses evolve. Put simply, a mutated virus that results in a variant is like a “faulty spell-check,” according to Yale Medicine.
“New versions (or variants) are a consequence of viral reproduction – each time a virus reproduces there is a chance for error in the assembly of the genetic material,” Jenifer Allsworth, a professor of medicine at the University of Missouri-Kansas City, told Flatland. “These mistakes result in variants. Most variants function the same as the original virus, but occasionally the genetic changes in the virus result in differences in how the virus behaves.”
More recently, Kamal Singh, a biochemist and virologist at the University of Missouri, said viruses mutate, depending upon what pressure they are under. In the omicron variant, the antibodies were unable to bind as well – or build that protective layer – to block the virus.
“Even one change in the protein where it is supposed to bind, it can completely abolish the binding,” Singh said. “I would say (that is ) one of the reasons at least omicron doesn’t care about vaccination.”
He and a team of researchers studied the omicron variant and identified the reasons why this particular variant bypasses antibody protection. Their study can be found here.
Q: What are the ABCs of virus mutations and what can we do?
In August, when the delta variant was of concern, Dr. John Fried, an infectious disease expert, told Flatland that variants are the result of a virus learning and mutating.
“Viruses mutate when they replicate and begin to divide,” Dr. Fried said.
When they divide, they take on different behaviors.
The key to curb infection, experts urge, is to get fully vaccinated and boosted as well continue mitigation strategies such as good hygiene, social distancing, avoiding crowded indoor areas and masking in public spaces.
For folks who are planning on traveling, testing is encouraged.
Watch this four-minute video to understand how mutations happen:
Q: Do vaccines protect against the omicron variant?
The short answer is yes. The vaccine will protect an individual against severe infection and, at times, hospitalization.
Physicians, virologists and epidemiologists caution against thinking this variant is mild and urge folks to get boosted or vaccinated as soon as possible.
Pfizer announced in December that three doses of its vaccine “neutralize the omicron variant (B.1.1.529 lineage)” while two doses offer some protection, but there’s still a chance for infection. This is normal.
Pfizer’s chair and chief executive officer Albert Bourla explained in a news release:
“Although two doses of the vaccine may still offer protection against severe disease caused by the omicron strain, it’s clear from these preliminary data that protection is improved with a third dose of our vaccine,” Bourla said.
In sum, boosters are important to fully protect against severe illness.
Listen to our KC Media Collective partner KCUR’s Up to Date episode on the variant, what to know and what experts say.
Jenifer Allsworth, associate professor of biomedical and health informatics at the University of Missouri – Kansas City’s department of medicine, helped weigh in on some topical questions folks might have about holiday or vacation travel and emergency services.
The following includes her responses to several of your questions.
Q: Should I wear a mask if I’m fully vaccinated and boosted? Why or why not?
“The current recommendations for mask use are vaccination status and situation dependent,” Allsworth said. Her key takeaways are:
- “The Centers for Disease Control and Prevention recommend masking in indoor public places for everyone 2 years or older who is not fully vaccinated.
- In outdoor settings, mask use is not currently recommended for those not fully vaccinated, unless the outdoor setting is crowded, includes close contact activities with people who are not fully vaccinated, or occurs in an area with a high number of COVID-19 vases.
- Individuals with certain medical conditions or medications that weaken the immune system are encouraged to follow the precautions recommended for unvaccinated people, including the use of a well-fitted mask.
- For people that are fully vaccinated, the CDC recommends indoor mask use in areas of substantial transmission of COVID-19.
Q: If I’m unvaccinated, what’s safe to do?
“With the rates of new COVID-19 increasing in most states across the U.S., unvaccinated or partially vaccinated individuals are at risk of contracting COVID-19. Unvaccinated individuals can protect themselves by following the CDC masking guidelines, using a high-quality, well-fitted mask, and selecting safer activities, including outdoor activities. When at an indoor activity, unvaccinated people can choose well ventilated locations, maintain social distance of 6 feet.
For smaller and family gatherings, both vaccinated and unvaccinated people can also use over the counter rapid self tests (FDA approved tests linked here.) to identify those most likely to transmit virus to others.
There has been considerable confusion about the reliability of self-tests for COVID-19 since they are a public health tool and not a diagnostic test.
Rapid self-tests are excellent at answering the question, ‘Am I infectious right now?” and interrupting transmission.”
Q: What should I know about visiting family and safety protocol?
“The best way to ensure a safe holiday is to get vaccinated and encourage unvaccinated family members to do the same. During family gatherings, we can reduce the risk of spread by following CDC’s recommendations for mask use, maintaining social distance, avoiding crowded and poorly ventilated indoor spaces, wash or sanitize hands and use rapid self-tests to determine infectiousness.
Q: Is it dangerous to see my family’s newest family member or our older family members or friends? Any tips on keeping them safe?
“To protect our most vulnerable family members we can follow these same recommendations – get vaccinated or boosted, adhere to the CDC mask guidelines, wear a well-fitted mask, choose safer locations for gatherings, practice hand hygiene and use rapid self-tests that answer the question, ‘Am I infectious?’
Q: If I’m healthy, do I need a booster? Why or why not?
The current recommendation is for everyone aged 16 and older who is 2 months (Johnson & Johnson) or 6 months (Pfizer-BioNTech or Moderna) after completion of the primary COVID-19 vaccination(s).
Q: Can prepared food carry COVID if it was in a home where people have the virus? How long do COVID germs stay on objects like dishes, doorknobs, etc.?
Currently, there is no evidence linking prepared food or food packaging to COVID-19 transmission.
“Most of SARS-CoV-2 transmission is believed to be the result of respiratory droplets that can remain airborne and detectable for up to 3 hours. While significantly less common, it is possible to contract the virus by touching plastic or stainless steel surfaces. The virus can be detected on these hard surfaces for up to 3 days.”
Q: Does the second dose of COVID vaccine cause shingles?
Shingles is caused by the varicella-zoster (chicken pox) virus that remains in the body in an inactive state. The virus can be re-activated by any stimulus to the immune system.
The COVID-19 vaccination, along with stress, the common cold, flu or any illness, could serve as the stimulus that reactivates the virus. Reports of shingles after vaccination have been extremely rare among the millions of people vaccinated in the United States and scientists have not been able to establish that these reported cases of shingles are linked to vaccination.”
Read our full Flatland report addressing this topic.
Q: Is it safe to go to the ER if I’m feeling sick?
“Yes! COVID-19 has had dramatic effects on healthcare and emergency rooms have been on the frontlines throughout the pandemic. While it is understandable that people are concerned about the ER, facilities employing proper safety and sanitation practices are safer than ever.”
Q: What advice do you have for people who feel ill if hospitals or ERs are full?
“For non-emergencies, reach out to your healthcare provider or local clinic/hospital for guidance. The COVID-19 pandemic has resulted in a dramatic increase in healthcare alternatives like telemedicine. For emergencies, call 911.”
“For non-emergencies, reach out to your healthcare provider or local clinic/hospital for guidance. The COVID-19 pandemic has resulted in a dramatic increase in healthcare alternatives like telemedicine. For emergencies, call 911.”
Q: Which age group is seeing a larger share of COVID-19 cases?
Data point to the young kids.
The Centers for Disease Control and Prevention’s (CDC) most recent data (last updated Aug. 30) shows a higher amount of COVID-19 cases among kids 12 through 17 years old. Children 5-11 are right behind them.
See the graph below to show the breakdown:
Children account for nearly 15% of cases nationwide as of mid-August and the cases continue to rise exponentially, according to the latest American Academy of Pediatrics report.
Children’s Mercy Hospital recently reported that 11 children were hospitalized, which included three in the intensive care unit.
Q: How do we keep our children safe if they’re going back to school?
This one is harder to answer because we’re still figuring this one out.
But to help control the spread, pediatricians, public health officials and science communicators recommend that children wear masks and socially distance themselves when around others outside of their household and in large congregate settings, like a classroom.
One Missouri-based epidemiologist recommends families employ what she calls a “protective bubble,” according to a St. Louis Public Radio report that appeared in KCUR.
How? Vaccinations. If parents are protected, they can protect their children from the more contagious variant. That’s important since hospitals are seeing more and more younger kids with worse COVID-related infections.
Even schools are looking for ways to help keep kids safe.
The rising number of cases in school settings have school administrators worried. Some have even begun to rethink their back-to-school plans, as our own Nick Haines reported this morning.
Several Kansas school districts implemented mask mandantes to help curb transmission.
Q: Can vaccinated people spread the virus if they experience a breakthrough case?
Yes, which is why public health officials recommend wearing face coverings in public settings or if in crowded areas.
“For people infected with the Delta variant, similar amounts of viral genetic material have been found among both unvaccinated and fully vaccinated people,” according to the Centers for Disease Control and Prevention’s latest update on the Delta variant transmission.
However, the CDC is still studying symptomatic and asymptomatic spread among fully-vaccinated people. As it stands now, the CDC’s research shows that vaccinated folks may shed the virus for a shorter period of time. This means the vaccine is properly equipping the body to fight against the invader pretty successfully.
With the body ready to fight, the virus has a lesser chance of infecting or causing complications.
Q: Is Ivermectin a safe way to fight off COVID-19?
No, medical experts warn. Ivermectin, an antiparasitic drug typically used on animals, has been cause for concern lately, according to the Kansas Reflector.
For one, it is not approved by the Food and Drug Administration. Secondly, it’s typically used to treat animals – not humans – against parasites.
But it isn’t safe for human consumption, despite disinformation spreading online. Simply put, ivermectin is not an antiviral medication and can do more harm than good.
Q: Can vaccinated people be infected with the Delta variant?
Yes, but the risk of infection is low. Studies show that the Delta variant of COVID-19 is more contagious than the previous strain. That means the virus can transfer from one person to the other more efficiently. So, what can you do?
The key here is to get both doses if you’ve chosen to get Moderna and Pfizer. You’re fully protected 14 days after getting it.
The Centers for Disease Control and Prevention (CDC) sounded the alarm in a July 16 news briefing, stating that there’s been a 70% jump in cases compared to the previous seven-day average. The Delta variant is spreading fast. We reached out to local experts to better understand what this means for us in the metro.
Dr. John Fried, an infectious disease physician at St. Joseph Medical Center, wants folks to understand that no vaccine is 100% effective.
The good news is that the vaccine reduces chances of infection and hospitalization by a large percentage. Vaccinated people who’ve tested positive for COVID-19 are less likely to develop severe symptoms and be hospitalized.
But folks should still be vigilant if they plan to congregate in public settings.
Dr. Fried said hospitals have seen an increase in COVID-19 patients in the past month and estimate that roughly 80% of patients are unvaccinated. Among the remaining 20%, most only received their first dose.
In terms of resuming medium- to high-risk activities such as going to restaurants or social gatherings without masks or social distancing, Dr. Fried said, “with the Delta you really need to wait after the second” dose.
Q: What happens if you’re fully vaccinated and get COVID-19?
Some experts say that fully vaccinated people who contract the new strain of COVID-19 may experience less severe symptoms.
The CDC recently published a report of an outbreak in an Oklahoma gymnastic facility, which sheds light on the patterns other public health officials have warned about. This report showed that a very small percentage of vaccinated persons were infected with the Delta variant, whereas the majority who were hospitalized were unvaccinated or had received one dose of Moderna or Pfizer. This means that the immune system has not yet been fully equipped to ward off the virus.
This aligns with Dr. Fried’s experience. He said the majority of patients in Kansas City area hospitals with the new strain of COVID-19 were unvaccinated or had just received their first dose.
Q: What does it mean that 38% are fully vaccinated or 44% of Kansas City residents are half vaccinated with the first dose?
Technically speaking, only 38% of the population is protected against severe infection or hospitalization, whereas 44% have gotten their first dose of the vaccine.
Those who are half vaccinated still have some protection against COVID-19. But they only will be considered fully vaccinated two weeks, or 14 days. after getting their second dose. By then, the antibodies that teach the body to fight the virus are in full effect.
The low vaccination rates in the metro area are concerning to public health officials because this increases the chances of the virus spreading in vulnerable communities.
Q: Will the city shut down if cases continue to rise?
Physicians and public health experts say shutdowns are less likely to happen. Though the cases are rising, the vaccine technically replaces shutdowns as a mitigation tool.
Plus, the shutdowns have accelerated other public health emergencies such as substance use disorder, and mental health-related illnesses such as anxiety, depression and suicide.
The goal when shutdowns were enacted was to curb the spread and vaccines do that. Not only do they reduce chances of getting severely ill, but they can also reduce transmissibility.
“Vaccine prevention is better than trying to mitigate the damage,” Dr. Fried said. “The energy should really be getting more people vaccinated.”
Q: Cases are rising but deaths aren’t as high as they were a year ago. Why is the uptick in cases concerning public health officials?
As of July 16, the cases in the Kansas City metro have nearly tripled in the past 30 days, according to the Kansas City Department of Health.
The numbers are nearing the count from February 2021, according to Kansas City’s COVID-19 Dashboard.
For Marynia Kolak, a health geographer at the University of Chicago, a rise in cases means the virus is not being contained. Kolak leads the COVID Atlas Project, which crunches data from the CDC, county public health departments and other research, combined with spatial analysis to create a map to show vaccination rates, COVID-19 rates, as well as poverty and other health data to put the health risks into perspective.
“COVID is not happening in a vacuum and the conditions that already existed in (different) counties can and do influence COVID outcomes,” Kolak said.


She pointed to the clusters of cases happening around Springfield, Missouri. Back in April, the data — thought spotty — showed signs of a pattern. Over the next few months, the cases began to spread to the north and south of the Kansas City metropolitan area.
During a walkthrough of the platform, Kolak hovered over the Midwest and showed how the map gradually turned red.
“We tend to find that these outliers, they don’t get checked,” she explained. “(They) start to kind of turn into red and then those red areas get bigger and bigger and bigger and you can really see that expansion happening in real-time.”
The Kansas City area includes a lot of commuters, so folks are constantly traveling from one state to the next, and from one county to another. Add an infectious virus to the mix and it’s a recipe for an even worse public health crisis.
Kolak and her research director hope to empower the public with tools like the COVID Atlas. They can search and find the information they need to make informed decisions.
Q: Are vaccines safe for children?
Yes. The Pfizer vaccine has been deemed safe and effective for children 12 years of age and older. Physicians and public health officials have been recommending vaccinations for children ever since the Emergency Use Authorization went into effect in May.
Q: How do we stop these variants from spreading and mutating?
Dr. Fried’s simple advice: Get the vaccine.
“Sure you might be fine but what about the poor kid with leukemia or grandma? We need to do this so we can all be safe,” he said.
Viruses mutate when they replicate and begin to divide. It’s a natural part of the process, he explained.
Most mutations are bad for the virus and most die, he said. But every now and then a mutation may affect one of three critical characteristics of the virus:
- how contagious it is;
- how aggressive it is, or what’s the mortality and morbidity because some viruses cause milder disease/severe disease;
- and resistance to various interventions like vaccines and antibodies.
“The best patriotic thing to do is not get infected,” Fired said. “That’s the only way to prevent mutation.”
Q: Is it safe to stop using a mask when in public?
The Centers for Disease Control and Prevention (CDC) recently announced that it’s safe to unmask if you’re fully vaccinated against COVID-19.
The CDC’s interim recommendations posted on May 13 stated: “Fully vaccinated people no longer need to wear a mask or physically distance in any setting, except where required by federal, state, local, tribal, or territorial laws, rules, and regulations, including local business and workplace guidance.”
But confusion sparked by that update has resulted in a flurry of news reports about what this means and what rescinding mask mandates was really meant to do.
An NPR report tapped behavioral experts to better understand the rationale behind the CDC’s decision to drop the requirement of masks for — and this is key — vaccinated people. They said the idea is to prompt folks who are hesitant or wary about getting the vaccine to consider signing up for the shot.
So, if you’re fully vaccinated it’s safe to unmask at work, depending on your company policy, and in most public places.
If you’re not, keeping a mask on will help prevent you from spreading disease to those around you, particularly those who are immunocompromised such as folks on chemotherapy and those with other chronic conditions.
Although most local governments quickly followed the CDC’s lead in dropping mask requirements, it is still unclear how companies and stores will regulate who’s vaccinated and who isn’t. Local public health officials are considering this issue at the moment.
Mask update: On July 28, Mayor Quinton Lucas reinstated the indoor mask policy effective Aug. 2 through “at least 12:01 a.m. on Saturday, August 28,” according to the news release. This means everyone 5 years old and older – regardless of vaccination status – should remain masked up in public areas.
On July 16, 10 Missouri county health departments issued a joint public health advisory that advises unvaccinated folks to remain masked in certain areas.
Recently, Missouri has led the nation in most cases per capita so both vaccinated and unvaccinated individuals are urged to exercise caution.
The advisory states:
- “Currently, only 40% of Missourians are fully vaccinated. Please assume that 1 in 2 people in any crowd or gathering may be unvaccinated. If you do not know the vaccination status of those around you, resume social distancing of at least six feet.
- If unvaccinated, being in crowds like restaurants, bars, fitness centers, or movie theaters puts you at a higher risk for COVID-19. Avoid indoor spaces that do not offer fresh air from the outdoors as much as possible.
- Additionally, continue practicing good hand hygiene by washing your hands frequently for at least 20 seconds.”
According to the news release, this is their guidance for folks who are not immunized currently:
“Unvaccinated individuals should wear a mask while visiting indoor public places, in crowded outdoor settings, and for activities with close contact with others who are not fully vaccinated.
- Be aware that people with underlying medical conditions may not be able to receive full protection from the vaccine and that children younger than 12 are not yet eligible for vaccination. These populations are vulnerable to being exposed to COVID-19.”
Q: Why are some states scaling down on vaccine shipments?
Simply put, not enough folks were getting vaccines at local clinics and mass vaccination sites.
At some point this spring, vaccines were being tossed out if they weren’t being used.
Kansas City PBS executive producer Nick Haines, host of “Kansas City Week in Review,” recently shared that some states, including Kansas and Missouri, are asking the federal government to cease sending large shipments of vaccines.
“This past week, the state of Kansas asked for less than 9% of its approved allotment from the government. The state currently has a stockpile of almost 647,000 doses,” Haines wrote on May 10.
Q: How close are the vaccines to getting full Federal Drug Administration (FDA) approval?
COVID-19 vaccines were first administered under what’s known as “emergency use authorization.”
In early May 2021, Pfizer and vaccine partner BioNTech started the application process to get full FDA licensure, according to NPR. The vaccine was fully approved in August 2021, and now available to everyone 16 years and older.
How long did it take to get there? Applications require six months worth of data to be considered and can take another six months to gain full approval.
“The (Biologics License Application) BLA submission is an important cornerstone of achieving long-term herd immunity and containing COVID-19 in the future,” said Ugur Sahin, M.D., CEO and Co-founder of BioNTech in a press release.
Experts explain the only difference between emergency use authorization (EUA) and full approval is that the folks involved in clinical trials are observed for longer.
In December 2020, the FDA issued an emergency use authorization for the Pfizer-BioNTech vaccine after an international study of 37,586 people.
According to the administration, “Part of FDA’s evaluation of an EUA request for a COVID-19 vaccine includes evaluation of the chemistry, manufacturing, and controls information for the vaccine.”
The FDA and CDC will continue to monitor vaccine safety after it’s been approved. Protocol dictates that all side effects should be monitored and evaluated to ensure all possible risks are identified.
Q: Does the FDA’s stamp of approval mean vaccines are more safe to get?
The vaccines were safe before full licensure. No corners were cut, say federal officials who have been on the front lines of vaccine development.
“These vaccines were developed without cutting corners or sacrificing our standards,” Dr. Peter Marks with the Center for Biologics Evaluation and Research (CBER) said in his recent congressional testimony on May 11.
The only thing that was fast-tracked was the paperwork and red tape. Vaccines are determined safe once slated for emergency use authorization, a rigorous process that requires a committee’s investigation of how clinical trials went and what the results were.
Q: Are vaccines safe for pregnant and breastfeeding people?
According to the CDC, you can get vaccinated if you are pregnant or breastfeeding.
People who are pregnant or breastfeeding are at a higher risk for developing a severe case of COVID-19 in comparison to non-pregnant people, and the vaccine can mitigate this risk. Clinical trials of the vaccine’s effect on pregnant people are still underway, and it is recommended that those who are pregnant or breastfeeding talk to their doctor before getting vaccinated.
According to the CDC website, “CDC and the Federal Drug Administration (FDA) have safety monitoring systems in place to gather information about COVID-19 vaccination during pregnancy and will closely monitor that information. Early data from these systems are preliminary, but reassuring. These data did not identify any safety concerns for pregnant people who were vaccinated or for their babies.”
Q: How will businesses know who is vaccinated? Can they ask?
Those who are fully vaccinated are now allowed to unmask in many settings, but how does anyone know who is vaccinated?
Some have been citing The Health Insurance Portability and Accountability Act of 1996, or HIPAA, as a valid reason to not share health information such as their vaccination status. This has been debunked.
Despite a widely held misconception, businesses and individuals do not actually fall under the category of entities regulated by HIPAA. This means that they are allowed to ask about your vaccination status and it is not a violation of the law.
Although businesses are allowed to ask for proof of vaccination, the new masking policies essentially amount to the honor system.
Q: What do I need to know about the J&J vaccine?
On April 12, 2021, federal regulators paused the distribution of Johnson & Johnson vaccines out of “an abundance of caution.” This move is common when adverse effects are reported to the Centers for Disease Control and Prevention. On April 24, 2021, regulators lifted the recommended pause after a safety review and, which is the protocol if any rare side effects or adverse effects arise.
While blood clots are rare, according to the CDC, officials reviewed the cases of six women whose cases first raised concern. Food and Drug Administration officials say these types of reactions could point to a rare autoimmune reaction.
These six cases showed a rare combination of two things: a blood clot that prevents blood draining from the brain that can cause strokes; plus another condition where people have low platelet counts.
What we know:
- Clots were found in women between 18 and 48
- Of the six women who initially reported to have blood clots, one died and one is in critical condition
- Vaccine sites and pharmacies temporarily replaced the J&J vaccine with either Moderna or Pfizer during the pause
After the safety review, the CDC and FDA released a fact sheet for healthcare providers, found here, and issued more guidance for recipients and caregivers, which is found and downloadable here.
Q: Do I need to be worried about blood clots if I already got the J&J vaccine?
In short, no.
Experts say those who have already received the J&J vaccine needn’t worry. Around 0.000088% of people who received the J&J vaccine developed a severe blood clot — that’s less likely than being struck by lightning .
University of Kansas microbiologist in the pharmacy school Bill Picking helped further contextualize the issue:
“The active components of these vaccines are not in the system all that long (maybe days to a week or two) before being processed by the body. Once whatever might be responsible for the clotting is gone, I would think you’re in the clear. It’s still not clear that the vaccine is directly responsible for this.”
Q: How should I expect to feel after each dose?
Every body reacts differently depending on their immune response or other conditions. However, the most common side effects are a sore arm, redness and swelling. Other effects include fatigue, headache, muscle aches, chills, fever and nausea.
Remember, these are signs that the body’s immune system is working. It’s like working out one day and feeling sore the next.
Can I get COVID-19 from the vaccine?
No, the vaccines currently being distributed in the U.S. do not contain a live virus in them. Therefore, they cannot give you COVID-19.
Q: What about allergic reactions to the vaccine?
Allergic reactions are possible. Microbiology professor Bill Picking explained the vaccines and possible ingredients folks could have adverse reactions to.
“One of the things maybe people are allergic to can be the polyethylene glycol because there are documented cases of people being allergic to polyethylene glycol,” Picking said.
“You’re not allergic to mRNA,” he continued. “Our cells make tons of mRNA every day. If you were allergic to it, you’d really have a problem. Although they’re completely unrelated, there are certain autoimmune disorders that involve nucleic acids.”
He also broke down a few of the ingredients in the mRNA vaccines such as lipids, or phosphocholine. Lipids play key roles in our body’s health and disease.
“Based on the ingredients, I’ve got to believe that the adverse reactions are going to be rare,” Picking said.
Q: What does being fully vaccinated mean?
Being fully vaccinated means it has been two weeks since your second dose of the Pfizer or Moderna vaccines, or two weeks after your first dose of the Johnson & Johnson vaccine.
Q: What can I do once I’m fully vaccinated?
The Centers for Disease Control and Prevention says the following activities are safe to enjoy once fully vaccinated, or two weeks after your second dose:
- Visit inside a home or private setting with other fully vaccinated people without a mask
- Visit inside a home or private setting without a mask with one household of unvaccinated people who are not at risk for severe illness
- Travel domestically without a pre- or post-travel test
- Travel domestically without quarantining after travel
- Travel internationally without a pre-travel test depending on destination
- Travel internationally without quarantining after travel
The CDC also notes that people should not visit indoors without a mask with people who are at increased risk for severe illness. People who are at increased risk include people with certain illnesses such as cancer or chronic illnesses like asthma and people who are immunocompromised who may not be able to get vaccinated.
Some people who are immunocompromised cannot produce antibodies in response to vaccines. These folks are at increased risk of infection with no way of fighting against the virus.
Other people who are at an increased risk include older adults and pregnant people, according to the CDC guidelines.
The CDC also recommends continuing to avoid medium and large gatherings.
Q: How long will the vaccine protect me from COVID-19?
The latest research suggests that current vaccines will protect against the virus for at least six months. That’s for both Moderna and Pfizer.
Experts such as epidemiologists and virologists say its protection could last even longer. While there’s not a hard and fast timeline yet, they estimate we might need yearly vaccines much like the flu shot.
The good news is that for the next six-plus months following your vaccination, your body will be equipped to fight against the virus, reducing your chances of complications and hospitalization.
The Moderna vaccine has 94% efficacy and Pfizer vaccine has 95%, which means those who get the shot have a 94% or 95% lower risk of getting COVID-19. Boosters for all vaccines are now available.
Infectious disease experts monitor “breakthrough cases” – those who get the vaccines and still get COVID-19 – and recommend a booster shoot to increase protection. Breakthrough cases are to be expected, experts say, because vaccine efficacy isn’t 100%.
Q: How often will I need to get a vaccine?
Let’s break this down per vaccine, focusing on the two messenger RNA (mRNA) vaccines.
As mentioned earlier, we still don’t know how often we’ll need to get a booster shot. Pfizer and Moderna have studied distributing a third booster not only to keep the body protected from COVID-19 but also the variants.
Pfizer:
- Pfizer CEO Albert Bourla said in a press conference taped on April 1 but released on April 15 that a third booster would likely be needed within 12 months of being fully vaccinated. Update: Boosters are recommended at least five months after getting the first two doses.
Moderna:
- Similar to Pfizer, Moderna’s CEO also has said a third booster shot should be available later this year. Update: Boosters are recommended at least five months after getting the first two doses. Moderna is approved as a “mix and match” booster option for those who’ve received the single-dose of another version of the COVID-19 vaccine, according to the FDA.
Q: Why are there variants or different strains of sars-CoV-2? How does that happen?
It’s like survival of the fittest and evolution. Viruses naturally mutate and change over time.
But sometimes, other factors contribute to the way it mutates. When the virus jumps from one body to another, it’s invading and finding a way to thrive. The more it spreads, the more it’s able to learn different survival strategies.
The CDC explained what the coronaviruses are and how scientists identify them:
“Coronaviruses are named for the crown-like spikes on their surfaces. Scientists monitor changes in the virus, including changes to the spikes on the surface of the virus.”
This is nothing new and is normal. Take for instance the flu virus, which mutates every year. That is why we’re recommended to take the annual flu vaccine.
In the meantime, unvaccinated and vaccinated people should continue to be vigilant and protect themselves to interfere with the chances of the virus spreading.
Q: Where can I register to get the vaccine?
You can visit the Jackson County Health Department’s website, or call (816) 404-6456 to determine eligibility and schedule an appointment to get the shot.
For vaccines in Johnson County, Kansas, visit the Johnson County Health Department’s website, or call (913) 715-2819.
The Wyandotte County interest form can be found on their website.
Clay County has an up-to-date phone line offering vaccine information in the county: (816) 415-3250. You can also visit their website.
Platte County is asking its residents to fill out this survey if they are interested in getting the vaccine.
Douglas County has asked residents to submit this interest form. Officials will reach out to schedule the vaccine.
Q: Is the COVID-19 vaccine safe?
Yes. All available vaccines have been thoroughly studied to make sure they are safe and effective.
There is a chance you could experience mild side effects after receiving the vaccine. These are normal. The vaccine gives the body a recipe to boost immunity, so the side effects mean your body is adjusting and learning to fight off the coronavirus.
Jason Glenn, at the University of Kansas Medical Center, put it this way:
“(The vaccine is) wearing a jacket with the virus logo on it, but there’s no actual virus inside. That teaches the immune system to attack anything that looks like that without actually exposing you to the risk that you might catch the disease.”
Side effects can include swelling around the injection site, fever, chills and headaches. In extremely rare cases, people have experienced anaphylaxis (a severe allergic reaction). However, providers have medicine available to treat the reaction immediately. This is why you must wait 15-30 minutes before leaving after receiving the vaccine.
Q: What are the ingredients in COVID-19 vaccines?
According to the Food and Drug Administration, the ingredients for the Pfizer vaccine are: mRNA, lipids ((4-hydroxybutyl)azanediyl)bis(hexane-6,1-diyl)bis(2-hexyldecanoate), 2 [(polyethylene glycol)-2000]-N,N-ditetradecylacetamide, 1,2-Distearoyl-sn-glycero-3- phosphocholine, and cholesterol), potassium chloride, monobasic potassium phosphate, sodium chloride, dibasic sodium phosphate dihydrate, and sucrose.
According to the FDA, the ingredients for the Moderna vaccine are: messenger ribonucleic acid (mRNA), lipids (SM-102, polyethylene glycol [PEG] 2000 dimyristoyl glycerol [DMG], cholesterol, and 1,2-distearoyl-sn-glycero-3-phosphocholine [DSPC]), tromethamine, tromethamine hydrochloride, acetic acid, sodium acetate, and sucrose.
Q: What is the capacity situation in Kansas City area hospitals?
This data may be outdated. Please refer to state and county data for updated figures.
The Kansas Hospital Association’s most recent data from Feb. 8 show that as of that date, 25% of hospitals in the Kansas City metro expected a staffing shortage that week. This includes data from hospitals in the following counties:
- (In Kansas) Johnson, Leavenworth, Miami and Wyandotte
- (In Missouri) Bates, Cass, Clay, Clinton, Jackson, Lafayette and Ray.
According to Kansas data, there are 333 hospitalized patients with COVID-19 and 86 patients who are in the ICU who are suspected or confirmed COVID patients.
The data also show that there are just 28% of “adult staffed ICU beds available” and 25% of “all staffed inpatient beds available.”
On the Missouri side, it’s about the same. The Missouri Hospital Association’s COVID-19 dashboard data from Jan. 31 to Feb. 6 showed that around medical bed availability hovers at around 22% and ICU beds at 21%.
Back in November, another Flatland report spoke to Alex Garza, incident commander of the St. Louis Metropolitan Pandemic Task Force to understand the impact of staff shortages.
Garza said: “An analogy would be, I could have 100 buses, but if I only got one driver, I got one bus. … The rest are just taking up parking spots.”
However, it’s worth noting that as of Feb. 8, hospitalizations in Kansas City have decreased by 19%, according to the Mid-America Regional Council. As Nick Haines recently shared in his latest installation of Nick’s Picks, Kansas City reported the lowest number of COVID-19 cases since July.
Q: Is coronavirus airborne? Is it floating in the air so even on a walk do we need to wear a mask?
Yes, in October the Centers for Diseases Control and Prevention found that the virus is passable through airborne transmission. However, that doesn’t mean you need to worry about catching it just walking alone outside.
COVID-19 is passed through respiratory droplets, which everyone produces when they speak, sneeze, cough, sing, yell or exhale deeply. These droplets typically travel a few feet before they fall to the ground. When people are in close proximity these larger droplets can spread to others.
Smaller respiratory droplets can hang in the air for hours instead of falling to the ground, these are called aerosols. These can move around in poorly ventilated indoor spaces, spreading to other people in the area.
The ways to avoid this airborne spread include:
- Wearing your mask if you are in proximity to others.
- Avoid spending time in crowded indoor spaces.
- Maintain 6 feet of social distance.
- Wash your hands often.
- Don’t touch your face without clean hands.
- Meet people in outdoor settings.
- If you are in a place with poor ventilation, open a window if possible.
Q: Why are the U.S., the state, and the city governments not spraying like other countries are doing, like Korea or China, to kill the virus?
The EPA does not recommend using fogging, fumigation, electrostatic spraying or drones to help control COVID-19 unless the pesticide product has specifically been labeled to include disinfection directions for those.
The CDC recommends cleaning contaminated surfaces with liquid disinfectants to prevent the spread of the disease.
As data emerges, the EPA may consider allowing some disinfectant registrants to add directions for UAV (unmanned aerial vehicle) use to their labels. Chinese agricultural company XAG Technology has been testing using drones to spray disinfected to help fight the virus.
Learn more with Kansas City PBS’ continuing coverage and list of resources:
Here are some other questions we’ve answered:
We’re still accepting questions! Write to us below:
Vicky Diaz-Camacho covers community affairs for Kansas City PBS. Catherine Hoffman covers community affairs and culture for Kansas City PBS in cooperation with Report for America. The work of our Report for America corps members is made possible, in part, through the generous support of the Ewing Marion Kauffman Foundation.